Robotics in Surgery
Go Home the Same Day after a Robotic-Assisted Knee Replacement
Chad Mitchell, MD, FAAOS
November 14, 2023
Is it possible to have a robotic-assisted knee replacement and go home on the same day? Today’s advancements in technology, post-operative pain management, and blood loss management make it easy to avoid admission to the hospital and go home on the same day as the surgery. Not only are robotic-assisted knee replacement patients going home from the hospital on the same day, but many are now having the same surgery in surgery centers. That’s right. Many patients are avoiding the hospital altogether and having it performed in surgery centers. It is amazing to watch patients safely walk out of the recovery room and get into their car within a few hours of their knee surgery.
There are various protocols for making it possible for a patient to go home the same day after a knee replacement surgery, but these protocols all have the same basic concepts. These basic concepts include: minimizing blood loss, outpatient DVT (Deep Venous Thrombosis) prophylaxis, controlling pain while maximizing alertness, antibiotic prophylaxis, immediate range of motion of the operative knee, early safe ambulation, and outpatient physical therapy.
During surgery, tranexamic acid (TXA) is used to effectively minimize the risk of a blood transfusion after a knee replacement. This medication is usually administered intravenously or locally within the incision. It works by blocking the breakdown of clots within the incision, but it has not been associated with an increased risk of the bad clots known as deep venous thrombosis (DVT). Also, TXA significantly lessens post-operative bleeding complications which can complicate a patient’s knee motion following the procedure. In other words, TXA helps make early range of motion of the knee and early ambulation possible following surgery by preventing bleeding complications. TXA also has almost eliminated the possibility of a post-operative transfusion, so patient’s can safely go home the same day without worries of major bleeding.
Outpatient DVT prophylaxis has changed in recent years also. Baby aspirin (81 mg) taken two times a day has been effective DVT prophylaxis in joint replacement patients. This is an oral medication that is much less likely to cause bleeding than some of the other anticoagulants that are available. It is an easy to acquire over-the-counter medication.
One of the more significant medical advances allowing patients to go home the same day from a knee replacement is the outpatient post-operative pain management. A patient’s pain has to be managed in such a way as to allow the patient to be very alert following surgery. Nerve blocks before or after the surgery help with controlling pain without affecting alertness. Also, outpatient non-narcotic pain medications are a priority to help the patient use less narcotics. Narcotic medications are notorious for making patients drowsy and less alert, so many protocols have the patient use the non-narcotic pain medications first, and use the narcotics sparingly for breakthrough pain. If the patient is comfortable and alert in the recovery room, then the patient will be able to ambulate with a walker and go home safely.
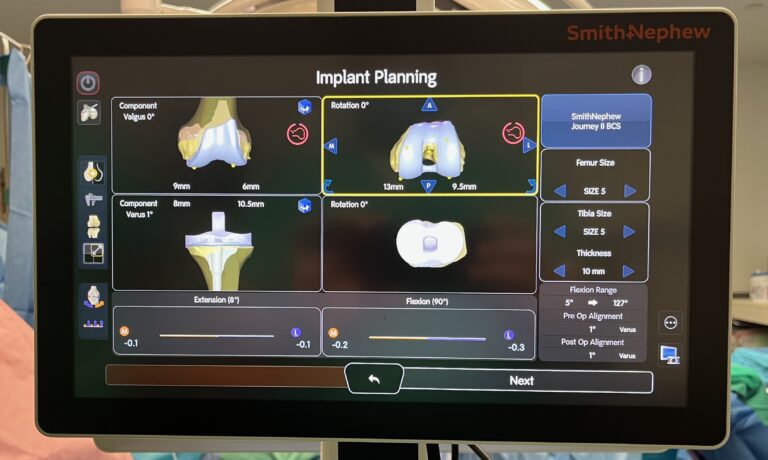
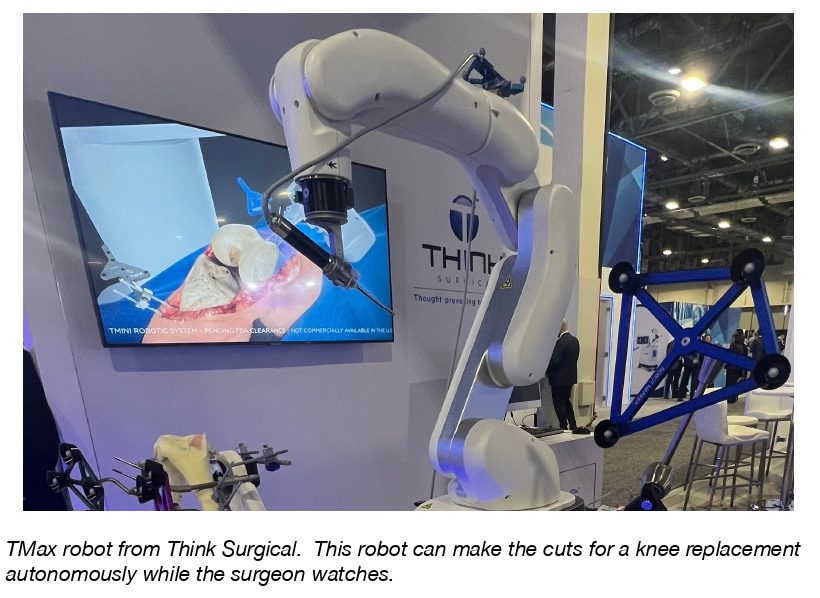
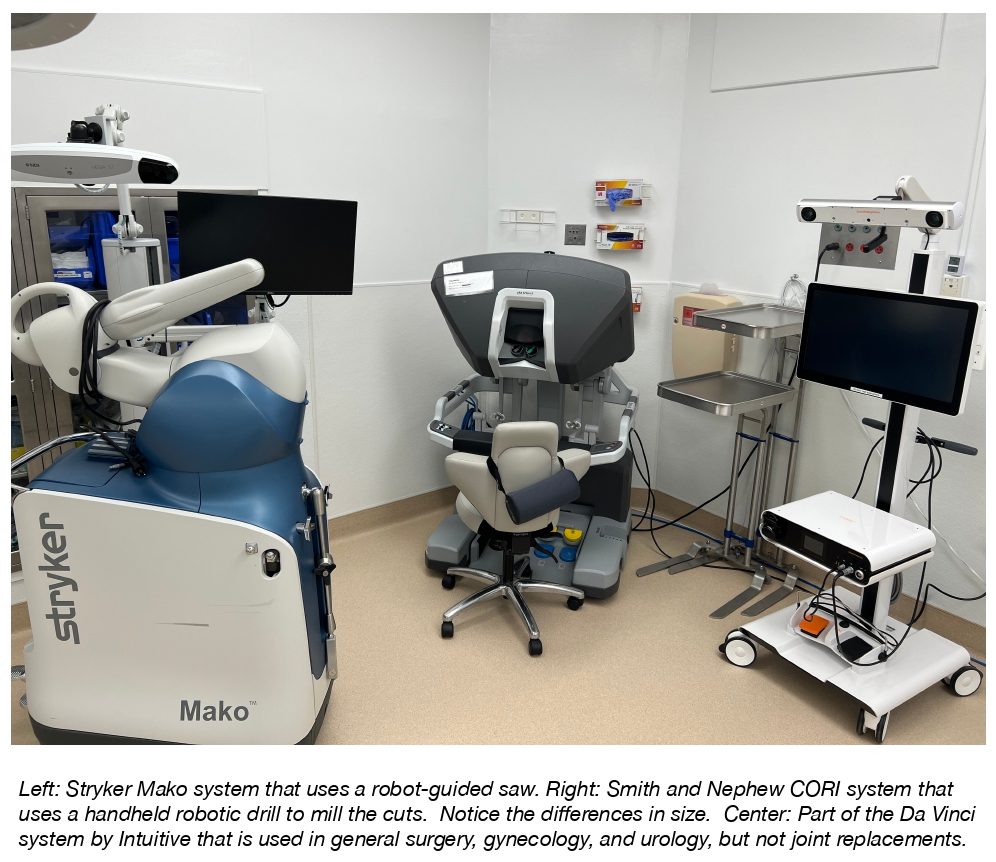
Robotics is also helping transform same day knee replacement surgery. The increased precision and alignment of the components of a robotic-assisted knee replacement allow better range of motion of a patient’s knee. Patients are able to go home on the same day and are finding it easier to maintain good range of motion in the days immediately following the knee replacement.
Outpatient physical therapy is usually prescribed to help patient’s maintain their knee motion during the healing phase when scarring can occur. Also, patient’s that have possible increased infection risks from diabetes and smoking can go home on oral antibiotics, in addition to the intravenous antibiotics given at the time of surgery.
In summary, patients are going home the same day from robotic-assisted knee replacements given many advancements in surgical and post-surgical care. Talk to your surgeon about this option if you are considering a knee replacement.